IBS/Focal Active Colitis
Dear Annie,
After a colonoscopy and several specialized tests, my doctors have diagnosed me with Focal Active Colitis. Unfortunately, he did not tell me anything else. He didn’t even explain what it is. The Doctor prescribed corticosteroids. But, after looking up the side effects, I decided that I would rather try a more natural route. Can you help?
Here is some background: I have been experiencing troublesome diarrhea for about a year and a half. I have had many tests, medication, and herbal supplements. Everything seems to work for a short time, then goes back to the way it was. There is some pain and cramping at times, but for the most part it is simply diarrhea. It comes on fast, often with no warning. Thank you for whatever information you can help with.
Thank you for reaching out. I imagine your frustrated and probably more than a little stressed. There is hope. Holistic medicine can be of great help in the management of colitis and IBS. However, there are a few things we need to talk about before we begin.
The following contains affiliate links. That means, when you click on or purchase a product through one of the links, I make a commission at no additional cost to you. Thank you for your support.
About holistic and herbal medicine as it pertains to long term and chronic conditions.
- There are no magic bullets. Treatment strategies will be most effective when applied individually and to the whole system. A multi-level approach works best with colitis.
- It may take several weeks to get things under control. Once you start a line of treatment, do not stop. This has been going on for over a year and may take at least 6 to 8 weeks to really notice a difference. If something isn’t working as you would like, talk to your practitioner so they can tweak your treatment strategies.
- Work with a natural health care provider such as a qualified herbalist, yoga therapist or naturopath. As you start to heal, your formulas, practices and diet may shift to meet your new level of wellness. The path to wellness, may take some turns and the protocol is likely to change during the healing process.
Now, let’s first begin with an explanation of Focal Active Colitis. Then we can go into treatment strategies and herbs that may be helpful.
About Focal Active Colitis
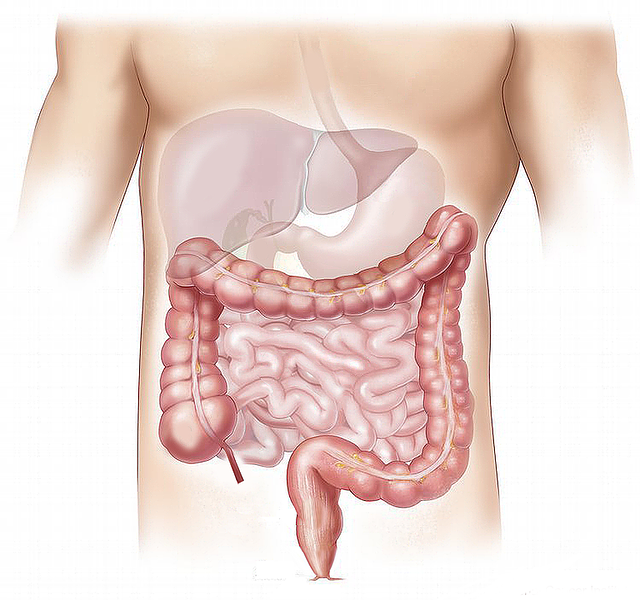
Focal Active Colitis is a type Inflammatory Bowel Disease (IBS). It is a type of colitis, or inflammation of the colon, in which there is an excess of inflammation affecting an intestinal gland called the crypt of Lieberkühn. Also called intestinal crypts, these are tube-like glands found in the lining of the colon and rectum. Colon crypt cells are responsible for making new cells to regenerate the lining of the intestine and make mucus.

Scientists think Focal Active Colitis (FAC,) along with some other types of colitis, is an auto-immune problem. That means that the immune system, designed to protect the body for outside invaders, becomes confused and begins to target healthy tissue, in this case the colon. In Focal Active Colitis, too many white blood cells are involved with the Lieberkühn crypts resulting in inflammation and dysbiosis or difficulties with the digestive tract including diarrhea, constipation, bloating, gas, pain, bleeding, and cramping. Symptoms can range from mild to debilitating.
FAC is most often grouped together with other forms of inflammatory bowel disease (IBD) and referred to as IBS or irritable bowel syndrome. Any kind of IBD can be a serious condition, one that requires a long-term and multi-level approach.
Causes of Focal Active Colitis
Experts do not know what causes FAC or any kind of IBS. They think genetics play a role. Onset of the disease may be triggered by an event or unusually high stress. The event itself is sometimes linked to an infection, accident, or a highly stressful situation. Further, symptoms or relapses seem to worsen at times of high stress.
Natural Strategies for Focal Active Colitis
When applying natural methods for treatment we will want to:
- Reduce diarrhea.
- Decrease inflammation in the colon.
- Support and vitalize mucus membranes.
- Encourage healthy reproduction of colon cells.
- Repair and support healthy gut microbiome.
Dietary Strategies
Diet plays a huge role in the management and possible resolution of FAC. Suggestions are broken into 2 stages. Stage 1 are recommendations for during the acute uncomfortable phase, when inflammation is present, and the problem is at its worst. Once symptoms have settled down and your feeling better, we move into stage 2 and can work toward your most optimal diet plan.
Stage One – Active uncomfortable symptoms and inflammation
- Reduce ruffage; limit course fiber. During active inflammation or flares it is best to avoid raw vegetables, including salad, lettuce, brown rice, etc. Instead, enjoy cooked vegetables, bone broth, cooked potatoes, squash, oatmeal, and well-cooked white rice. Too much fiber and ruffage can irritate the inflamed bowel.
- Add Ground psyllium seeds to water and drink 1 time per day. Studies show psyllium seed to be as effective as the medicine mesalazine for controlling symptoms or diarrhea, constipation, bloating, gas, cramping and pain.
- Choose mild, bland foods. Season lightly with ground turmeric, cumin, ginger, oregano, and other gut healing, digestive herbs.
- Cook all foods well.
- Add a probiotic supplement of between 75 and 150 billion cfu (colonizing forming units.)
- Eliminate major allergens from the diet including wheat, dairy, eggs, soy, nuts, and corn. Most people with IBD are gluten, lactose, and fructose intolerant. These 6 foods are implicated in a multitude of chronic issues ranging from IBS, arthritis, psoriasis and more.
- Stay grounded on this simple diet for 2 to 3 weeks, or until symptoms improve. Colitis can take up to 6 weeks to improve, even with medication.
- Journal your experiences. Strong emotions are not uncommon through this process. Especially as you eliminate foods that serve to buffer stress. Writing about your feelings, needs and experiences can help process underlying emotional issues or stress, thereby speeding healing.
Stage Two – Once you are feeling better
- Slowly add foods back into your diet. A good rule of thumb is to add 1 new food or substance every 3 to 5 days. This way you’ll know what foods cause problems and which are notorious and healthy for you.
- A high fiber diet supports gut microbiome, which supports healthy mucosa. Once the symptoms are significantly reduced, add small amounts of fiber at a time to your diet. Add slowly, paying attention to what your body likes or does not like.
- Avoid highly processed foods and food additives.
- Continue with probiotics or add fermented foods to your diet.
- Slowly add the allergens above, one at a time and watch for relations.
- Remain low sugar, fat, and alcohol.
The Mediterranean diet comes highly recommended for the treatment and maintenance of all types of IBS. Here is a link for more information about the Mediterranean diet and how to follow it.
Herbal Suggestions and Focal Active Colitis
In addition to diet and lifestyle modifications, herbs are used to address the underlying cause and to address symptoms. For our work with FAC, we will want to use the following types of herbs.
Anti-Inflammatory Herbs
Are applied to reduce inflammation. Herbs with a strong anti-inflammatory action that have proved helpful for irritable bowel diseases include Turmeric (Curcuma longa,) Boswellia serrata (also known as Indian Frankincense,) Ginger (Zingiber officinale,) Licorice Root (Glycyrrhiza glabra,) Echinacea root (E. angustifolia and purpurea root) and Andrographis paniculate.
Aloe vera gel, although not a strict anti-inflammatory, goes a long way to modulate the inflammatory response, especially in the gut. (Although it may be best used in stage 2. After acute symptoms have improved)
Immune modulators/immune amphoterics
Are used to normalize immune system activity. When the immune response is too high or too low, these herbs help the system find homeostasis or a healthy balance. Many of these herbs also have anti-inflammatory and antioxidant activity. They help soothe and heal involved nerve tissue, as well as protect the liver, kidneys, and nervous system.
Immuno-modulating herbs that may be appropriate for FAC include American Ginseng (Panax quinquefolius,) Licorice Root (Glycyrrhiza glabra,) Echinacea Root (E. angustifolia and purpurea,) and Andrographis paniculata.
Astringents/styptics
For Stage 1. Support the physical structure of the large and small intestines, help decrease or resolve diarrhea and stop bleeding. Herbs in the category include Myrrh (Commiphora myrrha,) Bilberry (Vaccinium myrtillus,) Rhodiola (Rhodiola rosea), Yerba Mansa (Anemopsis californica), Rose (Rosa spp,) Cinnamon (Cinnamomum verum,) and Red Root (Ceanothus americanus.)
Vulneraries
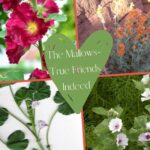
These plants heal, soothe, and protect the mucus membrane or the inside skin of the colon. They include Yerba Mansa (Anemopsis californica), Rose (Rosa spp,), Aloe Vera, Licorice Root (Glycyrrhiza glabra,) Chamomile (Matricaria chamomilla,) Turmeric (Curcuma longa,) Plantain (Plantago major,) and Calendula (C. officinalis.)
Alterative herbs
For Stage 2. Alterative herbs increase elimination of metabolic waste through the lymph system, bowels, kidneys, liver, skin, and respiration. At the same time, they help reduce oxidative damage and enhance the function of those systems. Many also have anti-inflammatory, antiviral, and antifungal properties.
For our purpose we will choose alterative herbs that promote healthy bowel function and flora like Dandelion, Yellow Dock, and Burdock.
Herbal suggestions for the treatment of Focal Active Colitis
True Solomon's Seal (Polygonatum multiflorum and other varieties)
Historically used to heal stomach and intestinal complaints, Solomon’s Seal works to decrease mucus discharges while adding a gentle tonic action. It acts as a mucilaginous tonic that is both tonic and restorative to mucus membranes of the entire digestive system. An excellent choice for the treatment of intestinal inflammation, chronic and acute dysentery (diarrhea), piles, or hemorrhoids and even worms.

Yerba Mansa (Anemopsis californica)
The roots and/or leaves of this lovely plant are gently astringent to help decrease chronic diarrhea. It supports and heals mucosal tissue (anywhere in the body), and serves as a useful antibacterial, anti-inflammatory and anti-viral agent. A lovely herb for our purpose.

Turmeric (Curcuma longa)
Whenever there is chronic inflammation with lower digestive involvement, I think of Turmeric root. It is an anti-inflammatory, and an immune modulator with antiviral, antifungal, antibacterial, antioxidant, and antineoplastic (prevents and inhibits tumors) actions. Turmeric aids every part of digestion, heals gut mucosa, and improves intestinal flora. The herb modulates the immune system, helps decrease metabolic toxins, stimulates circulation, and increases the absorption of nutrients by the colon.
For our purpose, use whole herb preparation or capsule, rather than those made with extracted constituents like curcumin. The suggested dose is ½ teaspoon Turmeric powder 2x per day.

Boswellia serrata (Indian Frankincense)
Also called Salai guggul in Ayurveda, Boswellia is a potent anti-inflammatory with documented success in the treatment of colitis. A 2015 study showed 70% of those diagnosed with ulcerative colitis that received 300 mg of Boswellia gum 3x per day achieved remission in 6 weeks. 88% of those with Crohn’s disease decreased symptoms significantly, which is a much higher percentage than for the groups receiving pharmaceutical medication or a placebo.
Licorice (Glycyrrhiza glabra)
Another great herb for our purpose is Licorice which is quite useful in the treatment of autoimmune diseases, including those of the intestines like IBD and Crohn’s disease. Used in Chinese medicine for centuries as a harmonizing agent, Licorice root is anti-inflammatory, adaptogen (helps the body deal with prolonged stress,) an immune modulator (helps regulate the immune system,) and hepatoprotective (protects and heals the liver.) It helps heal inflamed gastric and intestinal mucosa and inhibits the H. pylori bacteria, which causes most gastric ulcers.

Suggested dose is 1-2 ml of the tincture 3x per day. For the tea, make a decoction by gently boiling 1 tsp dried root in 10 ounces of water for 10 – 15 minutes. Then, cover and let the tea steep for 30 minutes. Drink 2 to 4 ounces 3x per day.
**Licorice is contra-indicated for those on steroid medications and by those who have high blood pressure.
Myrrh (Commiphora myrrha)
Astringent, digestive tonic, and carminative, Myrrh is indicated for the relief of chronic, long term diarrhea. It improves mucus membrane integrity, heals gut mucosa, helps stop bleeding or excessive fluid production and reduces inflammation and allergic response. Myrrh is effective in the treatment of leaky gut syndrome and mucus colitis (a very similar condition to FAC.)
Suggested dosage is 1 to 2 ml 4x per day.
Aloe Vera
Best used after diarrhea has been resolved, Aloe Vera is a cooling, soothing, anti-inflammatory, demulcent, anodyne (relieves pain,) vulnerary (heals wounds) and astringent. The juice or gel of the inner filet cools and sooths inflammation and limits damage of the stomach and intestines while stimulating healing of the intestines.
Fresh gel from the inner filet is best. However, I have had good results using a good brand of organic aloe juice, not gel. Be sure the only ingredients are aloe inner filet, water, and ascorbic acid (all commercial products have this.)

Recipes for Focal Active Colitis
Below are some possible recipes that may be helpful for those with focal active colitis or an active colitis flare. Remember that herbal remedies are best when they are formulated for specific people. They are not prescriptive and are not as effective when taken as a one-to-one replacement for pharmaceutical medication.
Nourishing Bone Broth and Veggies
This is a good recipe for initial stages of treatment when symptoms are at their worst. Nourishing bone broth heals, sooths and protects the gut while providing easy to digest protein.
- Choose 4 to 6 vegetables to work with. Avoid all nightshades including potatoes, tomatoes, eggplants, and peppers.
- Choose 2 organic meats to work with. For example organic Chicken, organic pork or organic beef.
- Use mild herbs for seasonings. May include onions, garlic, lemon grass, oregano, bay leaf, thyme, sage etc. Avoid hot or overly spicing food.
- May add rice or rice noodles.
- Organic bone broth may be purchased at the store or made at home.
To Prepare
- Use 1 quart bone broth
- 1 or 2 cups chosen meat, chopped and browned.
- add well chopped vegetables, onions, garlic and lemon grass (as is your choice)
- bring to a boil and simmer for a minimum or 20 minutes. (Or use a slow cooker).
- add spices
- Cook another 10 to 20 minutes until veggies are well cooked.
Enjoy.
Below is 1 idea that may work to decrease chronic diarrhea and inflammation associated with focal active colitis. In my experience, astringents tend to be more effective as a tea or infusion. Tinctures (herbal drops) can and will work, however they may not work as quickly.
To make an herbal tea place approximately 1 teaspoon of herb in 8 ounces of hot water and let steep for at least 20 minutes. Cold infusions (even better with astringents) can be made by adding room temperature water to the herbs and letting the set overnight.
Supportive Tea or Tincture
- 2 parts Yerba Mansa (Anemopsis californica) tincture
- 1 part True Solomon’s Seal (Polygonatum multiflorum) tincture
- 1 part Myrrh (Commiphora myrrha,) or Catnip (Nepeta cataria) tincture.
Suggested dose – 1 to 2 dropper fills of the tincture 2 or 3 times per day. Tea could be taken 1/3 cup 3 times per day.
- For more information about these formulas, product availability, or how to obtain personalized suggestions, contact Annie Jones here.
- For More information about Wonderment Gardens Products click Here.
Further Reading




Healing the causes of suffering – A four-step model for healing





















Thank you for reading. I hope you found this information helpful and interesting. Please do not hesitate to contact me if you have any questions. Also, if you have comments, please leave them in the comment section below. I would love to hear more about you and your experiences.
Many Blessings
Annie
References
https://www.nature.com/articles/nrc2392
Winston, David, AGH; Herbal Approaches to Auto-immune disease; Medicines from the Earth Botanical Conference notes, 2005
https://pubmed.ncbi.nlm.nih.gov/25830661/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3309643/
Winston, David, AGH; Herbal/Nutritional Gastroenterology; SWCBM conference notes, 2014
Stage, Katie, ND, AGH; Taming the Dragon, Botanical Approaches for IBD; Medicines from the Earth Conference notes, 2020.
Disclaimer
The statements and ideas presented here are not intended to diagnose, treat, cure, or prevent any disease or condition. They have not been evaluated by the FDA. All ideas presented are for the sole purpose of education. To help you take control of your own health. If you have a health concern or condition, consult a physician. We suggest that you always consult a medical doctor before modifying your diet, using any new product, drug, supplement, or doing any new exercises.
These statements and products have not been evaluated by the FDA. They are not intended to diagnose, treat, cure, or prevent any disease or condition. If you have a health concern or condition, consult a physician. Always consult a medical doctor before modifying your diet, using any new product, drug, supplement, or doing any new exercises.
Herbs taken for health purposes should be treated with the same care as medicine. Herbal remedies are no substitute for a healthy diet and lifestyle. If you are serious about good health, you’ll want to combine diet, exercise, herbals, a good relationship with your doctor and a generally healthy lifestyle. No one of these will do it alone.
This information is designed to be used as part of a complete health plan. No products are intended to replace your doctor’s care, or to supersede any of his/her advice or prescriptions.